Schizophrenia

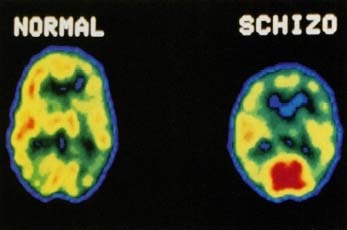
Schizophrenia (SKIT-zo-FREE-ni-a) is a complex, serious, and chronic brain disorder. It results from disruptions in the structure and function of the brain and neurotransmitter pathways of the central nervous system. These disruptions may cause psychotic symptoms, which are frightening distortions in thoughts, feelings, moods, perceptions, and behavior that interfere with daily life. With the correct combination of medication and therapy, the symptoms of schizophrenia often can be managed effectively.
KEYWORDS
for searching the Internet and other reference sources
Catatonia
Delusions
Hallucinations
Neuroleptics
Neurotransmitters
Psychosis
Information in the form of electrical signals flows down nerve cells in the brain, triggering the release of neurotransmitters. These chemical messengers transmit information from one nerve cell to another. In healthy people, neurotransmitter traffic usually flows smoothly, with occasional hills, valleys, bumps, and potholes that represent the stresses and challenges of growing up and interacting with other people. In people with schizophrenia, however, neurotransmitter traffic runs into major roadblocks, unscheduled stops, and unmapped detours to frightening and unreal places. These traffic disruptions result in periods of psychosis, during which people with schizophrenia lose touch with healthy reality and seem to get trapped in alternate realities. With anti-psychotic medication, people with schizophrenia often find their way back to the healthy realities of everyday life.
* chromosomes (KRO-mo-somz) are threadlike chemical structures inside cells on which the genes are located. There are 46 (23 pairs) chromosomes in normal human cells. Genes on the X and Y chromosomes (known as the sex chromosomes) help determine whether a person is male or female. Females have two X chromosomes; males have one X and one Y chromosome.
What Happens to People with Schizophrenia?
Neurotransmitter disruptions
Researchers know that in our chromosomes * are genes that direct the development of all the structures and functions of the brain and central nervous system, including the production and release of neurotransmitters. In schizophrenia, faulty genes may create coding errors affecting several different neurotransmitters. When those miscodings interact with environmental factors during childhood and adolescence, and even before birth, they may affect brain neurotransmitter levels and function, resulting in symptoms that doctors usually classify as positive and negative. Most often, the serious symptoms of schizophrenia do not appear until a person's late teens or early twenties.
Positive symptoms
The positive symptoms of schizophrenia are those that seem to distort and exaggerate sights, sounds, thoughts, perceptions, beliefs, and behaviors. People with schizophrenia usually do not experience positive symptoms until their late teens or early twenties, and doctors usually cannot diagnose schizophrenia before positive symptoms occur. The positive symptoms of schizophrenia may include delusions, hallucinations, and disorganized speech, thoughts, beliefs, movements, and behaviors.
- Delusions: Delusions are false beliefs that a person holds onto even when they are bizarre or could not possibly be true. Delusions may involve fears (paranoid delusions), guilt, jealousy, religion, spirits, one's role in life (delusions of grandeur), one's body, and mind control. People with schizophrenia might believe, for example, that their inner thoughts are being broadcast out loud or that outside people, spirits, or aliens are inserting thoughts into their heads or are touching their bodies.
- Hallucinations: Hallucinations involve seeing, hearing, or feeling things that are not real. People with schizophrenia often "hear voices" in their heads (auditory hallucinations) that other people cannot hear and that are not just their inner thoughts. The voices may tell them what to do, may carry on conversations about them, or may have arguments with each other.
- Disorganized speech, thoughts, and beliefs: People with schizophrenia may lose track of their ideas, meanings, and words ("word salad"). Ideas and images may become jumbled or linked together for illogical reasons, or words and meanings that should be linked instead may become disconnected.
- Disorganized movements and behaviors: People with schizophrenia may use exaggerated or repeated gestures, or they may seem to be fidgeting or hyperactive or preoccupied with meaningless physical movements.
Negative symptoms
The negative symptoms of schizophrenia usually involve a reduction in a person's normal level of functioning. People with schizophrenia may seem to think, speak, feel, and move less than healthy people do:
- Alogia (a-LO-jee-a) and poverty of speech: People with schizophrenia may speak very little, or their speech may have little meaningful content, or they may have long delays between words and sentences, as if the connections between thoughts and speech were interrupted or blocked.
- Flattening or blunting of affect: People with schizophrenia may have reduced emotional expression. They may not smile or frown in response to happy or sad events, their voices may not change tone or pitch, and they may not maintain eye contact or other kinds of emotional links with other people.
- Avolition and anhedonia: People with schizophrenia may seem to lose interest in and energy for pleasurable activities and achievements.
- Catatonia and posturing: People with schizophrenia may seem to freeze into unusual body positions, or they may seem to stop moving entirely.
Remissions and relapses
The negative symptoms of schizophrenia sometimes are seen during early childhood, when they may resemble autism and similar developmental disorders. By the late teens or early twenties, the positive symptoms of schizophrenia begin to appear. Mental health activist Ken Steele, for example, reported in The Day the Voices Stopped: A Memoir of Madness and Hope that his voices began when he was 14 years old.
Symptoms often occur in cycles, alternating periods of improvement (remissions) with periods of psychosis (relapses). Because schizophrenia is a permanent (chronic) disorder, it often gets worse as a person gets older, as periods of active psychosis interfere with perceptions of reality and activities of daily living. With the correct combination of medication and therapy, however, the positive and negative symptoms of schizophrenia often can be managed and controlled effectively.
The Genetics of
Schizophrenia
Scientists know that schizophrenia tends to run in families and that it affects both males and females, but they have not yet located the genetic coding errors that lead to the neurotransmitter disruptions that are seen in schizophrenia.
Studies of inheritance patterns show the following estimates of a person's risk of developing schizophrenia:
- 1%: general population
- 8%: when a sibling has schizophrenia
- 12%: when a parent has schizophrenia
- 14%: when a fraternal twin has schizophrenia
- 25%-35%: when both parents have schizophrenia
- 45%-50%: when an identical twin has schizophrenia.
Identical twins are siblings who develop from the same embryo. They always are the same sex and they share the same genetic material. If schizophrenia were entirely the result of a single genetic coding error, then the risk that identical twins both would inherit schizophrenia would be close to 100%.
Scientists believe that several different genes interacting with environmental factors is the likeliest underlying mechanism for schizophrenia. The U.S. National Institute of Mental Health has launched a Schizophrenia Genetics Initiative to gather data from people and families with schizophrenia. To find out more about it, check their website at www.nimh.nih.gov .
How Is Schizophrenia Diagnosed and Treated?
Diagnosis
The first step toward diagnosis is a complete medical examination and medical history. This helps the doctor to rule out other

Medications
Schizophrenia is considered a chronic disorder. There is not yet a "cure" for it, but there are medications that can offer relief from psychotic symptoms. These medications, called "antipsychotics," can help quiet the "voices" that interfere with daily activities and can result in dramatic improvements in the quality of life for people with schizophrenia.
Doctors must work very carefully with patients and their families to choose the right medication at the right dosage. When an effective medication is found, it often improves both the positive and negative symptoms of schizophrenia, reducing delusions and hallucinations and increasing social functioning.
Auditory Hallucinations and "Son of Sam"
During the 1970s, a man who called himself "Son of Sam" killed several people in New York City. When the killer was caught, he was identified as a man named David Berkowitz, who was having auditory hallucinations. In those hallucinations, Berkowitz heard the voice of a neighbor's dog (named "Sam") giving him orders to kill people in parked cars. Berkowitz still is in prison in New York.
Originally introduced during the 1950s, chlorpromazine (Thorazine) was the first medication used to treat schizophrenia. It was considered a "major tranquilizer" and it often produced unpleasant side effects. In the decades since then, researchers have discovered many newer medications that target malfunctioning neurotransmitters more accurately, improve symptoms more effectively, and cause fewer side effects. Newer medications introduced during the 1990s include clozapine (Clozaril), resperidone (Risperdal), olanzapine (Zyprexa), quetiapine (Seroquel), and ziprasidone (Geodon).
Medication dosages often require adjustments over time to maintain effectiveness or to reduce side effects. Sometimes people with schizophrenia stop taking their medication or stop checking in with their doctors, possibly because they feel better or because of unpleasant side effects from the medication. Without medication, however, psychotic symptoms are likely to return or worsen.
Side effects
Antipsychotic medications sometimes result in side effects that can make it difficult or distressing for patients to follow their doctors' recommended treatment plan. The older medications like chlorpromazine (Thorazine) often produced symptoms like sluggishness, emotional numbing, drowsiness, restlessness, muscle spasms or tremors, dry mouth, weight gain, and blurring of vision. A more serious side effect of long-term use of the older medications was a condition called "tardive dyskinesia" (TAR-div dis-ki-NEE-zee-a). People with tardive dyskinesia experienced involuntary movements of the face or arms or legs, movements that sometimes did not disappear when the medication was stopped. Often, people who developed tardive dyskinesia chose to continue taking their medication because the beneficial effects outweighed this serious side effect. It is important to note that each new generation of medications works more effectively than the older ones in relieving psychotic symptoms, reducing the severity of side effects, and reducing the risk of tardive dyskinesia.

Psychotherapy and support networks
As with other chronic diseases, people with schizophrenia need support from doctors, counselors, social workers, family, friends, and other people with the same disorder. Therapy can help people with schizophrenia learn how to accept their diagnosis, manage their symptoms and relapses, and adjust their daily lives to incorporate their medication and treatment plans.
Living with Schizophrenia
Once it was the norm for people with schizophrenia and other psychotic disorders to be hospitalized when they were diagnosed and to remain hospitalized for the rest of their lives. Today it is more common for patients to be hospitalized for only a short period of time, while their psychotic symptoms are being brought under control. As long as they remain on medication under a doctor's supervision, many people with schizophrenia are now able to remain at home with their families or in supervised group homes.
Dementia Praecox" and
"Schizophrenia": Emil Kraepelin
and Eugen Bleuler
Psychosis has been written about since before the time of the ancient Greeks, but the scientific study of mental disorders is still rather new in human history. Previous generations often believed that psychosis was a form of possession by supernatural spirits because people with schizophrenia seemed to "see things" and "hear voices" that were not real. Often people with schizophrenia and other psychotic disorders were put in prisons or in lunatic asylums.
It was not until 1896 that the German psychiatrist Emil Kraepelin (1856-1926) developed a classification system for mental illnesses in which he identified a group of psychotic symptoms that he called "dementia praecox" (de-MEN-sha PRAY-cox), from the Latin term meaning "precocious" or "premature" dementia. Kraepelin took note of many of the distorted thoughts and perceptions that signaled the start of the disorder, the age at which it seemed to occur most often, the periods of remission and relapse, and the fact that the disorder was chronic and usually got worse with the passage of time.
The Swiss psychiatrist Eugen Bleuler (1857-1939) later renamed the disorder "schizophrenia" from the Latin phrase for "splitting of the mind." Bleuler did not mean that people with schizophrenia had dissociative identity disorder ("multiple personality disorder") or "Jekyll and Hyde" personalities. Rather he meant that people with schizophrenia had minds that seemed to become fragmented and disrupted when they needed to coordinate thoughts, emotions, and behavior with the real world. Processes of mind that ran smoothly in healthy people instead seemed to split into fragments in people with schizophrenia.
Current research suggests that Bleuler was on the right track. As researchers identify the specific functions of the neurotransmitters that become disrupted in schizophrenia, the medications designed to target those neurotransmitters become more effective and cause fewer side effects.
Therapy for people with schizophrenia
Psychotherapy often helps people with schizophrenia learn to manage the behaviors that accompany psychotic symptoms and adjust to the rhythms and requirements of chronic illness. Therapy may involve a "token economy" technique that uses rewards for behavioral change. It also may involve rehabilitation and social skills training so that people with schizophrenia can catch up with the everyday skills and opportunities that had to be put on hold during periods of psychosis. Taking care of oneself, talking and listening during ordinary conversations, and interacting with friends, family, coworkers, and community in the real world all are skills that can be learned or relearned.
Family education
Family members also must learn how to overcome the confusion, shame, guilt, regret, grief, and stigma often attached to mental illness. Help in understanding the biology of schizophrenia is important, as is acceptance by family members that the signs and symptoms of schizophrenia are real and not just a way to avoid accepting reality and responsibility.
Family members must learn how to cope with specific symptoms like delusions and with alternating cycles of remission and relapse. People with schizophrenia are at a higher risk for depression and suicide, making it essential that family members know when to intervene and summon professional help. During periods of active psychosis, it usually is not helpful for friends and families to challenge delusions. But it is possible for them to communicate openly and honestly that they do not share the psychotic delusions even though they know that they are real for the person with schizophrenia.
Family members also play an important role in helping patients stick to their prescribed treatment plan. Patients with disorganized thinking may forget to take their medications, or their "voices" may tell them they do not need medication at all. At such times, family members who recognize the signs and symptoms of schizophrenia can take action to get immediate treatment, to prevent a relapse, and to keep the person with schizophrenia in touch with the reality of managing his or her disorder.
Resources
Books
Greenberg, Joanne. I Never Promised You a Rose Garden. New York: New American Library, 1984. Originally written under the pseudonym "Hannah Green" to protect the author from the stigma of mental illness, Joanne Greenberg's classic novel about a girl with schizophrenia was published in 1964 and has been in print continuously ever since.
Steele, Ken, and Claire Berman. The Day the Voices Stopped: A Memoir of Madness and Hope. New York: Basic Books, 2000. This moving autobiography tells the story of mental health activist Ken Steele, whose voices began when he was 14 years old and continued for decades until his doctors found the right medication to control his symptoms.
Organizations
U.S. National Institute of Mental Health, 6001 Executive Boulevard, Room
8184, MSC 9663, Bethesda, MD 20892-9663. This division of the National
Institutes of Health oversees research on schizophrenia and other mental
illnesses. It publishes the
Schizophrenia Bulletin
for researchers and many helpful fact sheets for the public.
Telephone 301-443-4513
http://www.nimh.nih.gov
American Academy of Child and Adolescent Psychiatry, 3615 Wisconsin Ave.
NW, Washington, DC, 20016-3007. The American Academy of Child and
Adolescent Psychiatry website posts
Facts for Families
about schizophrenia and other psychiatric disorders.
Telephone 202-966-7300
http://www.aacap.org
National Alliance for Research on Schizophrenia and Depression, 60
Cutter Mill Road, Suite 404, Great Neck, NY 11021. This nonprofit
organization supports scientific research on brain and behavior
disorders.
Telephone 516-829-0091 or 800-829-8289
http://www.narsad.org
National Alliance for the Mentally Ill (NAMI), Colonial Place Three,
2107 Wilson Blvd., Suite 300, Arlington, VA 22201-3042. This
information, advocacy, and support group for people with mental illness
and their families and friends sponsors a self-help education program
called
Living with Schizophrenia and Other Mental Illnesses (LWS).
LWS programs currently are active in more than 30 states.
Telephone 800-950-NAMI or 703-524-7600
http://www.nami.org
American Psychiatric Association, 1400 K Street NW, Washington, DC,
20005. An organization of physicians that provides information about
schizophrenia.
Telephone 888-357-7924
http://www.psych.org
National Mental Health Association, 1021 Prince Street, Alexandria, VA
22314-2971. A nonprofit organization that addresses all aspects of
mental illness and health and supports education and research to improve
mental health.
Telephone 800-969-6642 or 703-684-7722
http://www.nmha.org
National Mental Health Consumers' Self-Help Clearinghouse, 1211
Chestnut Street, Suite 1207, Philadelphia, PA 19107. This organization
makes information available to consumers about various mental health
issues, including mental health services and resources.
Telephone 800-553-4539 or 215-751-1810
http://www.mhselfhelp.org
All other \" Theories \" are now rejected. Therefore all other possible \" Facts \" are also rejected.
Certainty is present even though the \" Illness \" is not fully understood. This is NOT possible without error, or insanity, for certainty requires completeness.
Therefore, the mental illness to be studied, is that suffered by those whom have achieved this false certainty that also claims others are having false beliefs.
The problems will be overcome once false certainty is eliminated.
Thanks
But my opinion is the same. There are no bounderies, then how can it be said what is normal and what is not? We should conform knowing that what is abnormal today will be considerd normal tomorrow? Maybe?
Let's just throw a bunch of things that seem unconventional as symptoms. Mental illnesses are stigmatized(gasp!) then why taking it so lightly?
In a naive way I must say: All persons don't think the same, some are different from anothers,some people have problems for it, some are fine with it. Why do we always have to execrate, being hypocrat with the borders